Dementia is commonly seen as a disability “strik[ing] at the cognitive capacities which are central to our identities and our sense of self”.
As a result, the way people with dementia are treated by others around them often reflects that they are ‘lost causes'. They are considered completely unable to reconcile their identity which once existed, and now exist “increasingly devoid of content, an unbecoming of the self”, some theorise.
Even though it is undeniably true that elements of one’s selfhood are deeply affected during the progress of dementia, I’ve often found it to be a strange and problematic opinion to think that people with dementia are no longer themselves in any capacity, because of their inability to remember certain events and people in their life.
This perspective implies that selfhood, our notion of identity, is inextricably linked to our cognitive capacities. Believing this means one must accept that people diagnosed with dementia necessarily stop becoming themselves because they suffer from a disease that targets these very capacities which many consider essential to maintaining any degree of self.
Let’s call this opinion the ‘Cognitive Bias’ — an opinion that the self only exists in one’s cognitive capacities.
I’m not denying the real tragedy that accompanies someone with dementia being almost completely incapable of remembering their loved ones, but our attitudes and perceptions of people with dementia can end up making things a whole lot worse.
I guess the first question we need to clarify here is:
What is the self?
To find out why the Cognitive Bias view of the self might be prevalent, maybe the first place to go is by looking at some philosophers involved in the field of personal identity. It appears that some of the most influential agree that one’s notion of self is necessarily and exclusively linked to one’s cognitive capacities.
Locke is quoted here, saying;
“…a thinking intelligent being […]; which it does only by that consciousness which is inseparable from thinking, and, as it seems to me, essential to it…’”.
Here, he at least implies a view of selfhood that entails that our identities are constituted by the memories and experiences we have, which is sometimes called the ‘psychological continuity theory of personal identity.
For example, what makes Jim the same person numerically from age 6 to age 60 (despite undergoing many life changes), are a chain of memories that link together for him to retain and realise his identity.
If we are to refer to Jim’s personal identity as the main constituent of his selfhood, then it’s clear why this view is taken into considerations of dementia.
If Jim is diagnosed with dementia affecting his cognitive capacities, meaning he is unable to recall pivotal moments of his life (like the day he graduated with his Archeology degree in the 70s, or the moments where he befriended some of the closest people in his life), it seems reasonable to conclude that his conception of self has been significantly reduced.
According to this basic interpretation of Locke’s view, if Jim’s chains of memories are broken due to the degeneration of his memory, he is no longer the same Jim.
This implies that his identity is irrevocably altered, and Jim post-dementia assumes a new identity that makes him a different person. Perhaps in some people’s eyes, he is a ‘lesser’ person to the one he used to be due to disruptions in this chain of memories that constitute Jim’s identity.
Locke’s view of psychological connectedness as the only way to understand the self has faced criticism in philosophical circles. Regardless, there are still strong adherents to his theory among psychologists, scientists and care practitioners, who settle on this psychological connectedness view of the self.
This involves the implication that people with Alzheimer's and dementia are not identical to the people who occupied their bodies before radical memory loss, reinforcing the Cognitive Bias.

Why is this a problem?
If we agree with the Cognitive Bias, then our default response to people with dementia is likely to consider them as ‘less than people’. As a result, the recently acquired wishes, desires and interests of people living with dementia are patronised, and we can stop any remaining self from expressing itself and being validated.
Where Jane used to love writing before she received her dementia diagnosis, and now post-dementia Jane takes an interest in watering the flowers or painting, these new hobbies might be considered as not her “real interests” by the people around her. It is likely to be seen as a coping mechanism rather than a hobby, to keep herself occupied in the midst of her degenerating mind.
But just because Jane isn’t interested in writing due to her degenerating cognitive capacities, and has taken a liking to a hobby that appears ‘simpler’, it doesn’t mean she enjoys it any less.
A few years ago, I volunteered at a dementia care home to investigate the care and treatment provided to people with dementia. Although generally, there were good measures in place to treat people with dementia with humanity, it still appeared carers had to continuously remind themselves to avoid ‘malignant care’ — a term coined by Kitwood to describe carers treating them more as dementia patients, rather than people.
Whether it be ignorance or refusal to respect the preferences of people with dementia so carers can look after them — like force-feeding food they don’t enjoy to ensure they don’t starve — these attitudes and actions significantly encroach their autonomy, and limits the ability of people with dementia to express their identity through their preferences.
Some carers claimed to ‘know what’s best' for people with dementia and often responded to their worries with deception to make them feel safe and at ease. But despite good intentions, this attitude is counter-productive.
Just as much as you don’t have an appetite for carrot and lentil soup today, neither does someone with dementia. Dementia has nothing to do with an individual’s will and desires, but because they are perceived to no longer be themselves, they are treated as if they have already lost everything it means to be human.
Continuously thinking of people with dementia in this way means they will also eventually perceive themselves as completely ‘gone’ because identity is not just your own perception of yourself. A great deal of it is constituted by the way others recognise and perceive you.
More disastrously, it neglects other elements of selfhood that are still operating in someone with dementia. Denying these elements might very well be the reason someone completely loses themselves, and that’s the harm we are doing to them — rather than dementia itself.

Have any attempts been made to change this?
Certainly, it’s not an unpopular opinion that people with dementia are habitually mistreated. Kitwood’s ‘Personhood’ movement was particularly influential in challenging pathological dementia care in the 1990s, by strongly advocating a person with dementia’s state of well-being, which demands comfort, inclusion, attachment and trust.
Personhood is strictly defined as; “a standing or status that is bestowed upon one human being by others”, emphasising the importance of dementia care practices recognising people with dementia as just that — people who require social interactions, respect, and freedom of choice just like anyone else.
Kitwood emphasised a notion that selfhood can be found in places completely unrelated to one’s biological capacities, such as the friendships and social interactions we make throughout our lives.
In fact, elements of the self are always revealed in social interactions with others. Even if people with dementia cannot recall faces, they remain children, mothers and fathers with inseverable family ties.
Though Kitwood’s work was a step further in refuting the Cognitive Bias, it might have been too successful. It may have inadvertently privileged a social conception of the self over other things that constitute the self, which still lives on with people with dementia.
In other words — although Kitwood’s great work re-emphasised that people with dementia still have an identity irrespective of their condition, there are other ways the self lives on within people with dementia that we must recognise.
If we choose to accept one explanation of what the self is and where it might be, we ignore everywhere else it might be. This is certainly not a price we ought to pay when considering the lives of people with dementia. So it begs the question:
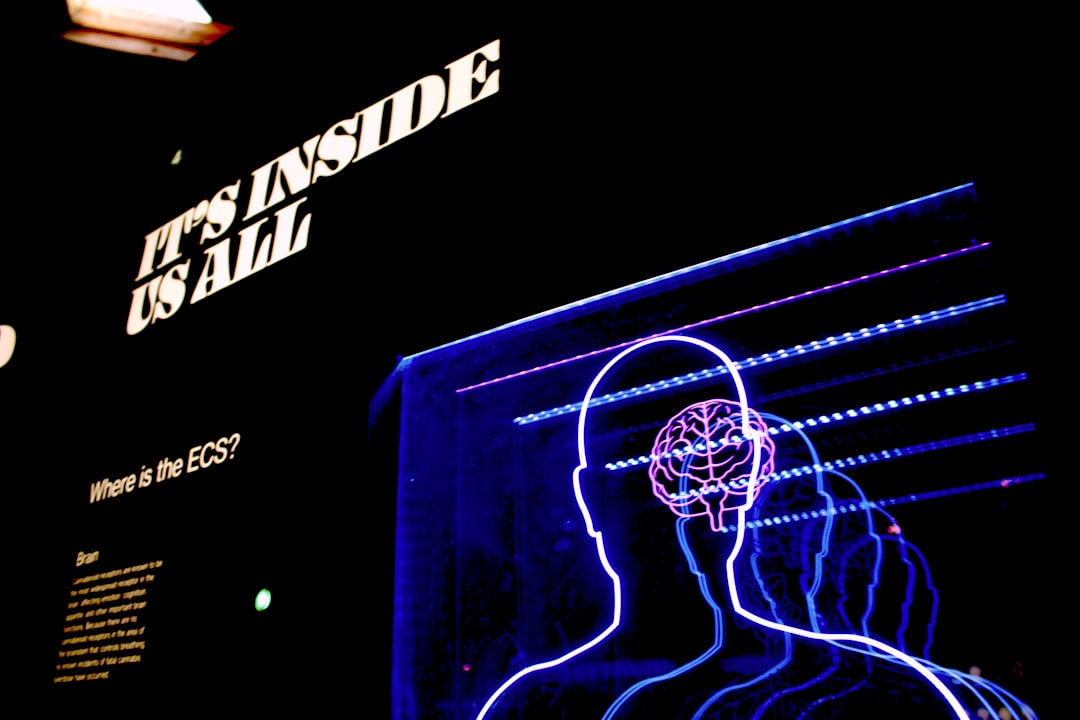
If selfhood is not just constituted in the mind or social structures, where else might it be?
A field of philosophy called phenomenology prioritises the first-person, lived experience as a way to understand reality. It gains conclusions not by relying on studying and measuring reality via scientific methods, but by taking into account what we can know from our everyday experience of life.
So another place we could find a conception of self that doesn’t rely on the brain is by comprehending the first-person experience of people with dementia. Some theorists in the field particularly focus on the body.
Pia Kontos advanced a notion of selfhood that is essentially ‘embodied’, finding her ideas in Merleau-Ponty’s conception of the pre-reflective body. Her idea suggests that a self that exists in the body, “beneath the threshold of cognition”, and independent of the brain.
We won’t get too deep into Merleau-Ponty’s theories of the body. But for the sake of discussion, he posited ideas that certain ‘motor skills’ (bodily actions), habits and cultural mannerisms can be performed without the need for conceptual thought, and therefore exist in the body.
That might sound ridiculous, but when we loosely refer to muscle memory (like driving a car without consciously thinking about shifting a gear before turning the wheel or walking, in the same manner, you did when you were a kid), that’s what Merleau-Ponty means when talking about the “pre-reflective body’s capacity for knowledge”.
Another good example is typing. When I type a word, I am pressing multiple buttons with letters to spell out a given word. But I am not consciously thinking about every single letter I press; it is as if my body autonomously performs these actions whilst my brain conjures a sentence to articulate.
This is promising news for people living with dementia. Despite the loss of memory and cognitive capacities, there is indeed a self that has been cultivated over the years through one’s body.
Learned motor skills that people with dementia have, such as non-verbal communicative activities like dancing and playing instruments, to the unique characteristics and mannerisms expressed in distinct cultural ways like eating with one’s hands, strikingly reveal a self that ought to be explored further in dementia care.
Kontos herself claims that an embodied approach to dementia care should take into consideration things we take for granted, like;
“The way that persons with dementia unthinkingly carry and project their bodies with coherence; the often subtle attentiveness to their appearance, cleanliness, and social etiquette; bodily expressions of class distinction; and the spontaneity of their actions”.
It is difficult to deny that even the subtlest expressions of self are still revealed in people with dementia, and so the self lives on despite living with dementia! The question now is:
How can these alternate understandings of self affect the treatment of people living with dementia?
So far, we have demonstrated that mind-independent conceptions of selfhood do indeed exist, such that a person living with dementia still inhabits a self. Phenomenology has pointed us towards the body as a reasonable residence of identity.
This leaves space for a plethora of exciting and innovative possibilities for the treatment of people living with dementia.
Yet the present reality is that they are not often theoretically considered or practically implemented, entailing the possibility for the bodily self in people with dementia to be ignored.
If this is permanently left unchecked, as I’ve said before, it could lead to a complete and faster loss of self which could have been otherwise avoided.
Taken what we know now, let’s explore three activities and events which primarily incorporate the bodily self in people with dementia, with the aims of not only revealing a strong sense of self but help people with dementia solidify and realise this more in care practices.

Improving Care Centre Environments To Feel Less Hospital-y
An imperative element of incorporating a bio-phenomenological approach to dementia care involves an understanding of how bodily behaviours are responses to environments, which therefore involves paying significant attention to the scenery and settings of care centres.
Reed-Danahay investigated this subject, and posited a distinction between ‘non-lieu’ (non-place) and ‘lieu’ (place) in care centre environments, where non-lieu is reminiscent of pathological care environments involving bland coloured walls, distinct ‘hospital smells’ and generally environments that resemble office spaces rather than comfortable homes.
Instead, we should strive for alternative ‘lieu’ settings in care centres which “facilitates connection, enhances memory and fosters identity”.
Kontos argues that emphasis should be placed on “maximising bodily coherence” in care centres, giving an example of how care centres could be divided by activity engaged in the room, like having a dining room that resembles one found in a home, or a ‘sleeping room’ which includes comfortable pillows and beds soliciting relaxation.
Because the body becomes a fundamental means of engaging with the world due to cognitive impairment, environments should take great care and attention in ensuring the setting is inviting for people with dementia to exercise bodily actions (like dancing) and reminds them of familiar ‘homely’ settings.
The bodily self is more likely to express knowledge in the pre-reflective body when perceiving environments where they were once learned. If Susie learned how to paint canvases in her living room next to a big window watching her garden when she was in her 20s, then simulating this environment in care centres is more likely to allow Susie to exercise her motor skill of painting more effectively.
Dancing
Dancing is a common effective activity practised in dementia care centres that inadvertently adopts a bio-phenomenological approach to selfhood in dementia — by incorporating the pre-reflective body to engage in movements and expressing one’s self in unique movements with others.
It is a powerful form of therapy that unwittingly demonstrates several key aspects of a bio-phenomenological approach to dementia care; it encourages a proprioceptive awareness of the body (dance movements emphasise awareness that one is embodied), expresses unique socio-cultural mannerisms in a fun way, involves an intersubjective element with others which makes it as a communal activity, and has an affective dimension that reconnects people with dementia to old memories they have forgotten.
“it provides a uniquely powerful insight into what it means for us to be ‘body-subjects’ — body-knowers and body-expressers — wholly human”.
A proprioceptive awareness of the body reinforces many of Merleau-Ponty’s ideas, as it demonstrates how one has an immediate sense of their body other than our five senses of vision, touch, scent, taste and sound.
It provides information regarding the ‘internal’ senses of our body — such as fatigue, hunger, balance, and the position of our limbs relative to one another.
Such awareness is independent of cognitive capacities; people with dementia still retain an internal sense of the position of their limbs relative to one another and express this when dancing to music.
The fact they are naturally able to shuffle their feet and appropriately respond to the rhythm of whatever song is playing demonstrates that they have this proprioceptive awareness, and in even advanced demented states, indicates that their pre-reflective body (and a self) remains functional.
Having regular dance sessions at dementia day centres reinforces this awareness of the body so much so that it serves as a reminder for people with dementia that they are still embodied and identify with their bodies — encouraging them to feel comfortable with themselves and their condition.
When I was working at a care centre, dancing was a regular activity that showcased the unique movements of all the people with dementia characteristic of sociocultural upbringings — from the way the old English women tended towards a bashful curtsy, to the way an Ethiopian man with dementia would move their shoulders in an Eskista fashion.
Purser highlighted the phenomena of dancing as something essentially social; “not only does the dancer reflect that movement to the other, but the other then reflects the dancer’s movement to the dancer”.
It demonstrated how dancing involves much more than an awareness of one’s body, but also necessarily involved a social dimension where dance movements are mirrored between people.
I also witnessed this exact phenomenon at the care centre.
Different bodies were communicating with each other through dancing, mirroring the same dance movements and sometimes performing complex dance movements in unison. It fundamentally demonstrated an expression of the pre-reflective body, not just on an individual level, but also having efficacy to communicate with other pre-reflective bodies.

Finally, dancing is an action naturally performed in one’s body in response to certain types of music, exemplifying an emotive dimension. It has the potential to reconnect people with dementia to memories they may have forgotten, by playing specific songs from significant eras of their lives, pervading them with joyous nostalgia.
I recall a man who was severely demented at the daycare centre who was not enthused by any activity occurring and remained seated for most of the time I was there. However, in the afternoon when the carers put on a dance session, they played Sweet Caroline by Neil Diamond which remarkably sprung the old man from his seat, who recognised it as his wedding song and performed a tender dance perhaps reminiscent of the same movements he did at his wedding.
This struck me as dancing being a surprisingly effective way for people with dementia to not only express their bodily selves, but access lost memories and actions in their pre-reflective bodies when responding to music that had a significant emotional impact on their lives.
It follows that dancing which significantly incorporates the body becomes another instance in questioning the strong influence of the Cognitive Bias in dementia care.
It follows that dancing which significantly incorporates the body becomes another instance in questioning the strong influence of the Cognitive Bias in dementia care.
Non-Verbal Communicative Activities
Finally, encouraging non-verbal communicative activities like cooking and creative arts may be beneficial for people with dementia.
Providing they have previously learned a motor skill such as learning the guitar when perceiving a guitar, they need not rely on cognitive capacities entirely to play it but can rely on their muscle memory to have their fingers in particular positions on the fretboard to strike a chord.
Or if they have previously cooked delicious recipes day after day, it is likely they can still access this knowledge in their bodies and slice butter or crush walnuts in a particular way to bake a cake.
Encouraging non-verbal communicative activities not only provides a means for the bodily self to express itself but brings about a host of other benefits devoid of pre-existing pathological care.
It can be fulfilling for people with dementia to perform motor skills like playing the guitar and painting in helping them reconnect with themselves (especially if it was a passion for them), and is one way that necessarily respects their autonomy — by giving them control over their self-development and assisting them in realising goals they want to pursue.
Pursuing arts, in particular, can be therapeutic in relieving anxieties and agitations caused by the condition, and cooking provides an opportunity to expose characteristic recipes from individual backgrounds.
Both activities can also be communal, providing the potential for people with dementia to foster friendships and relationships in performing these activities.
Wrapping it up
There’s no denying that our attitudes towards disabled people, in general, can be damaging towards their selfhood, especially when we consider them to be ultimately disadvantaged and unable to participate in many of the same activities as someone able.
The way others recognise us constitutes our identity in very real ways, and if we deny disabled people the ability to express their self in any way, then in the particular case of dementia, there is no wonder that we (and they) perceive them to have completely lost themselves.
We express ourselves all the time without realising it, and it is only by overthinking what this ‘self’ is, do our confused notions of selfhood arise and harm ourselves and others around us. People with dementia are of course, more vulnerable in this respect than your average joe.
Finally, I just want to acknowledge the sensitivity of this subject to those who have family and friends living with dementia. I appreciate it is challenging for some to see where I am coming from when a loved one might be in a progressive stage of dementia, and proposing this argument might appear to trivialise one’s personal experiences with their loved ones.
I also do not mean to condescend or devalue the hard work that carers put into dealing with the lives of people with dementia, it is a difficult job many of us lack the perseverance to do. But by criticising the ways of the past, can we find promising solutions for the future.
I write this with optimism, purely to help us all see people living with dementia as still people with selves, and suppose that the future of dementia care should strive to be more creative, rather than purely scientific.